Difference between revisions of "What is the History of Contact Tracing"
(→Early History) |
m (Admin moved page What is the History of Contact Tracing? to What is the History of Contact Tracing) |
||
| (12 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
| − | Contact tracing is | + | __NOTOC__ |
| + | [[File:4-Figure2-1.png|thumb|left|Figure 1. John Snow's results in a cholera outbreak in London helped to pin the outbreak to a specific pump. ]] | ||
| + | Contact tracing is a system designed to determine how diseases are transmitted from person to person. Contact tracing has been used extensively during the COVID-19 pandemic. Contact tracing involves tracking individuals who may have come into contact with infected individuals who have been infected with a virus or bacterial infection. | ||
| − | + | While technology, particularly mobile phones, is seen as the key to making modern contact tracing work, in the past other forms of contact tracing were employed. Much of the current approach to contact tracing is based on the historical development of this idea. | |
| − | Contact tracing | + | ====Early History==== |
| + | Contact tracing is not new. It has developed over the last two hundred years, but we have historical evidence of partial attempts to trace the infections in the past. The earliest recorded evidence comes from the Medieval period, during the Black Death plague, individuals who had the plague were not only quarantined, but their homes were marked. Often a cross or marker would be put so that everyone would know that a given house should be avoided. | ||
| − | + | These markers were an early attempt to contain local outbreaks by helping those around an area where someone became infected to know they should avoid contact. This mark, of course, would have created problems for the infected individual, often sealing their fate, but it could potentially limit the spread of the outbreak. The main problem was there is no evidence any systematic mapping of infected individuals was practiced. | |
| − | + | One of the earliest efforts to map an outbreak of infection comes from John Snow, who helped track and map the source of a cholera outbreak in London in 1854 (Figure 1). His work dismissed the idea that 'foul air' spread cholera and other infectious diseases. When he mapped the location of the infected individuals, it became clear that the source of the infection was a district in Soho London. Snow was even able to trace the illness to a particular water pump on Broad Street as the source of the cholera outbreak. | |
| − | + | Simply talking to people, finding out when and where incidents of infection occurred, and then mapping that data helped to create among the first maps of a disease outbreak. This work made him one of the key founders of epidemiology and public health. Soon after these outbreaks, London's sanitation improved, with the pump replaced, and with the work formed the basis of public health strategies that helped to diminish future outbreaks.<ref>For more on John Snow's work, see: Hempel, Sandra. <i>The Medical Detective: John Snow, Cholera and the Mystery of the Broad Street Pump</i>. London: Granta Books, 2007.</ref> | |
| − | |||
| − | + | ====Development of Public Health in the 19th Century==== | |
| + | Snow's work suggested that it was possible to track down the source of illness (not just Cholera) and track its spread. Early forms of contact tracing were applied to other infectious diseases as the late 19th century progressed. Tuberculosis (TB) was one of the biggest concerns during the rapid urbanization in the late 19th century. Cramped conditions and infected droplets made the spread of this disease rapid in the growing cities of Europe and North America. | ||
| − | + | By the 1880s, mandatory reporting of TB was required in the United States and Europe so that public health officials could map and trace the location of outbreaks. This effort created a system that could alert public health officials to warn people in affected areas that an outbreak was occurring. While response time was still relatively slow, which led to epidemics not being effectively contained, the fact that public officials mapped outbreaks helped. It allowed public health officials to identify areas where infected people needed to be isolated. By the 1880s, contact tracing was effectively developed as a primary public health strategy.<ref>For more on how contact tracing was used in the 19th century and TB, see: National Collaborating Centre for Chronic Conditions (Great Britain), and Royal College of Physicians of London. <i>Tuberculosis: Clinical Diagnosis and Management of Tuberculosis, and Measures for Its Prevention and Control</i>., 2006. http://www.ncbi.nlm.nih.gov/books/NBK45802/. </ref> | |
| − | + | ====Recent Developments==== | |
| + | [[File:smallpox-news.png|thumb|left|Figure 2. Smallpox was eradicated in large part due to contact tracing efforts by the WHO.]] | ||
| + | Contact tracing in the late 19th century was mostly related to the large-scale public health crises such as cholera or tuberculosis outbreaks. However, increasingly medical science in the early 20th century realized contact tracing has a positive effect on other forms of infections. Sexually transmitted diseases, which were not well studied prior to the early 20th century, increasingly were treated similar to other infectious disease. In Scotland and UK, during World War I and after, venereal disease became a public health concern. When contact tracing was deployed, it created many problems for those who were seen as passing the infections, mainly women, and the authorities. | ||
| − | + | In the 1920s and 1930s, contact tracing for venereal disease became common. Unfortunately, instead of using contact tracing for only public health reasons, it was instead used by authorities to track criminal activity such as prostituion. Additionally, it was used as a way to socially ostracise individuals. Public health officials began to see the problem with this approach change course in the 1930s and 1940s. | |
| − | + | Instead of emphasizing policy goals outside of public health, health officials switched a more robust focus on conducting detailed interviews with infected individuals and reconstructing the sexual history of individuals so that a more clear history of transmission could be developed. This effort was seen as vital during the war years in the 1940s because of the presence of more foreign and domestic soldiers in the UK during World War II. Nevertheless, contact tracing still restricted movements by infected or likely to be infected women, which was seen as the best way to prevent the spread of infection. | |
| − | ==References== | + | In the United States, in the late 1930s syphilis was seen as a potential public health threat. The United States Surgeon General ,Thomas Parran, promoted contact tracing as a way to prevent syphilis's spread. Initially, the program was difficult to accept socially and was also seen as a way for the authorities to control specific individuals, but by the late 1940s more controlled interviews and use of penicillin proved to be more successful than the earlier, blunter and more stigmatizing approach. These efforts helped diminish the number of syphilis cases by the 1950s in wide areas of the United States. <ref>For more on how venereal disease began to use contact tracing and controversies around this, see: Aral, Sevgi O., ed. <i>Behavioral Interventions for Prevention and Control of Sexually Transmitted Diseases</i>. 1. softcover print. New York, NY: Springer, 2008. </ref> |
| + | |||
| + | Perhaps the most successful example of using contact tracing to diminish the effects of a disease is the example of smallpox, which was mostly eradicated by 1980 (Figure 2). This was mainly due to efforts of contact tracing, by isolating and treating infected individuals, and then also focus immunization efforts for people nearby, thereby focusing available resources to those who most urgently need immunization. The World Health Organization (WHO) perhaps established one of the largest contact tracing programs that now focused on the entire world. From the 1950s-1970s, contact tracing was used in developed and developing countries, where teams of volunteers, doctors, and individuals would go and interview people to determine the likely place in which an outbreak was present. This helped to track all major areas of smallpox that eventually led to its near eradication. The combination of a vaccine and contact tracing made this among the most successful, large-scale WHO efforts.<ref>For more on the success of smallpox contact tracing, see: McGuire-Wolfe, Christine. <i>Foundations of Infection Control and Prevention</i>. Burlington, MA: Jones & Bartlett Learning, 2018, pg. 11. </ref> | ||
| + | |||
| + | ====Impact of Contact Tracing==== | ||
| + | Contact tracing has transformed public health and epidemiology since its inception. The most recent advances have to do with the use of mobile phone data. The 2014 Ebola outbreak and 2015 MERS outbreak shaped South Korea's and some other Asian countries' experience with a major viral outbreak. The use of mobile phones and tracing someone's whereabouts was used under powers issued to the government. This experience helped South Korea and other east Asian countries pioneer the use of such data to track how individuals movements may affect the transmission of an infectious disease. | ||
| + | |||
| + | While this was used initially in the Ebola and MERS outbreaks, the use in the 2020 COVID-19 outbreak proved essential for South Korea, China, and other east Asian countries in limiting the overall impact of COVID-19. While the use of mobile data for Western states is only now being applied, it also remains controversial given concerns over location data and personal data sharing with government authorities. Nevertheless, it is clear from the history of contact tracing, even without the use of mobile phones, tracking someone's whereabouts and the likely community in which they could spread the infection is critical in reducing infection rates. | ||
| + | |||
| + | The example of syphilis, cholera, tuberculosis, and smallpox all demonstrate this even without the use of mobile phones.<ref>For more on recent contact tracing technology and application, see: Mittelstadt, Daniel Brent. <i>The Ethics of Biomedical Big Data</i>. New York, NY: Springer Berlin Heidelberg, 2016, pg. 26.</ref> | ||
| + | |||
| + | ====Summary==== | ||
| + | Contact tracing has been seen as an essential public health strategy since the mid-19th century, when it was realized by John Snow that mapping infections and outbreaks could help reduce the overall outbreak or at least contain it. Public health officials realized this was not only true for cholera but using contact tracing for other infectious disease has proven useful in limiting their impact on the public. New technologies should allow more rapid response and tracing of individuals, helping to isolate local outbreak more rapidly before individuals infect a large number of people. | ||
| + | |||
| + | ====References==== | ||
| + | <references/> | ||
| + | |||
| + | [[Category:Wikis]] [[Category:Medical History]] | ||
Latest revision as of 22:56, 21 September 2021
Contact tracing is a system designed to determine how diseases are transmitted from person to person. Contact tracing has been used extensively during the COVID-19 pandemic. Contact tracing involves tracking individuals who may have come into contact with infected individuals who have been infected with a virus or bacterial infection.
While technology, particularly mobile phones, is seen as the key to making modern contact tracing work, in the past other forms of contact tracing were employed. Much of the current approach to contact tracing is based on the historical development of this idea.
Early History
Contact tracing is not new. It has developed over the last two hundred years, but we have historical evidence of partial attempts to trace the infections in the past. The earliest recorded evidence comes from the Medieval period, during the Black Death plague, individuals who had the plague were not only quarantined, but their homes were marked. Often a cross or marker would be put so that everyone would know that a given house should be avoided.
These markers were an early attempt to contain local outbreaks by helping those around an area where someone became infected to know they should avoid contact. This mark, of course, would have created problems for the infected individual, often sealing their fate, but it could potentially limit the spread of the outbreak. The main problem was there is no evidence any systematic mapping of infected individuals was practiced.
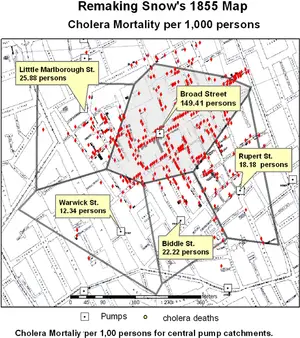
One of the earliest efforts to map an outbreak of infection comes from John Snow, who helped track and map the source of a cholera outbreak in London in 1854 (Figure 1). His work dismissed the idea that 'foul air' spread cholera and other infectious diseases. When he mapped the location of the infected individuals, it became clear that the source of the infection was a district in Soho London. Snow was even able to trace the illness to a particular water pump on Broad Street as the source of the cholera outbreak.
Simply talking to people, finding out when and where incidents of infection occurred, and then mapping that data helped to create among the first maps of a disease outbreak. This work made him one of the key founders of epidemiology and public health. Soon after these outbreaks, London's sanitation improved, with the pump replaced, and with the work formed the basis of public health strategies that helped to diminish future outbreaks.[1]
Development of Public Health in the 19th Century
Snow's work suggested that it was possible to track down the source of illness (not just Cholera) and track its spread. Early forms of contact tracing were applied to other infectious diseases as the late 19th century progressed. Tuberculosis (TB) was one of the biggest concerns during the rapid urbanization in the late 19th century. Cramped conditions and infected droplets made the spread of this disease rapid in the growing cities of Europe and North America.
By the 1880s, mandatory reporting of TB was required in the United States and Europe so that public health officials could map and trace the location of outbreaks. This effort created a system that could alert public health officials to warn people in affected areas that an outbreak was occurring. While response time was still relatively slow, which led to epidemics not being effectively contained, the fact that public officials mapped outbreaks helped. It allowed public health officials to identify areas where infected people needed to be isolated. By the 1880s, contact tracing was effectively developed as a primary public health strategy.[2]
Recent Developments
Contact tracing in the late 19th century was mostly related to the large-scale public health crises such as cholera or tuberculosis outbreaks. However, increasingly medical science in the early 20th century realized contact tracing has a positive effect on other forms of infections. Sexually transmitted diseases, which were not well studied prior to the early 20th century, increasingly were treated similar to other infectious disease. In Scotland and UK, during World War I and after, venereal disease became a public health concern. When contact tracing was deployed, it created many problems for those who were seen as passing the infections, mainly women, and the authorities.
In the 1920s and 1930s, contact tracing for venereal disease became common. Unfortunately, instead of using contact tracing for only public health reasons, it was instead used by authorities to track criminal activity such as prostituion. Additionally, it was used as a way to socially ostracise individuals. Public health officials began to see the problem with this approach change course in the 1930s and 1940s.
Instead of emphasizing policy goals outside of public health, health officials switched a more robust focus on conducting detailed interviews with infected individuals and reconstructing the sexual history of individuals so that a more clear history of transmission could be developed. This effort was seen as vital during the war years in the 1940s because of the presence of more foreign and domestic soldiers in the UK during World War II. Nevertheless, contact tracing still restricted movements by infected or likely to be infected women, which was seen as the best way to prevent the spread of infection.
In the United States, in the late 1930s syphilis was seen as a potential public health threat. The United States Surgeon General ,Thomas Parran, promoted contact tracing as a way to prevent syphilis's spread. Initially, the program was difficult to accept socially and was also seen as a way for the authorities to control specific individuals, but by the late 1940s more controlled interviews and use of penicillin proved to be more successful than the earlier, blunter and more stigmatizing approach. These efforts helped diminish the number of syphilis cases by the 1950s in wide areas of the United States. [3]
Perhaps the most successful example of using contact tracing to diminish the effects of a disease is the example of smallpox, which was mostly eradicated by 1980 (Figure 2). This was mainly due to efforts of contact tracing, by isolating and treating infected individuals, and then also focus immunization efforts for people nearby, thereby focusing available resources to those who most urgently need immunization. The World Health Organization (WHO) perhaps established one of the largest contact tracing programs that now focused on the entire world. From the 1950s-1970s, contact tracing was used in developed and developing countries, where teams of volunteers, doctors, and individuals would go and interview people to determine the likely place in which an outbreak was present. This helped to track all major areas of smallpox that eventually led to its near eradication. The combination of a vaccine and contact tracing made this among the most successful, large-scale WHO efforts.[4]
Impact of Contact Tracing
Contact tracing has transformed public health and epidemiology since its inception. The most recent advances have to do with the use of mobile phone data. The 2014 Ebola outbreak and 2015 MERS outbreak shaped South Korea's and some other Asian countries' experience with a major viral outbreak. The use of mobile phones and tracing someone's whereabouts was used under powers issued to the government. This experience helped South Korea and other east Asian countries pioneer the use of such data to track how individuals movements may affect the transmission of an infectious disease.
While this was used initially in the Ebola and MERS outbreaks, the use in the 2020 COVID-19 outbreak proved essential for South Korea, China, and other east Asian countries in limiting the overall impact of COVID-19. While the use of mobile data for Western states is only now being applied, it also remains controversial given concerns over location data and personal data sharing with government authorities. Nevertheless, it is clear from the history of contact tracing, even without the use of mobile phones, tracking someone's whereabouts and the likely community in which they could spread the infection is critical in reducing infection rates.
The example of syphilis, cholera, tuberculosis, and smallpox all demonstrate this even without the use of mobile phones.[5]
Summary
Contact tracing has been seen as an essential public health strategy since the mid-19th century, when it was realized by John Snow that mapping infections and outbreaks could help reduce the overall outbreak or at least contain it. Public health officials realized this was not only true for cholera but using contact tracing for other infectious disease has proven useful in limiting their impact on the public. New technologies should allow more rapid response and tracing of individuals, helping to isolate local outbreak more rapidly before individuals infect a large number of people.
References
- ↑ For more on John Snow's work, see: Hempel, Sandra. The Medical Detective: John Snow, Cholera and the Mystery of the Broad Street Pump. London: Granta Books, 2007.
- ↑ For more on how contact tracing was used in the 19th century and TB, see: National Collaborating Centre for Chronic Conditions (Great Britain), and Royal College of Physicians of London. Tuberculosis: Clinical Diagnosis and Management of Tuberculosis, and Measures for Its Prevention and Control., 2006. http://www.ncbi.nlm.nih.gov/books/NBK45802/.
- ↑ For more on how venereal disease began to use contact tracing and controversies around this, see: Aral, Sevgi O., ed. Behavioral Interventions for Prevention and Control of Sexually Transmitted Diseases. 1. softcover print. New York, NY: Springer, 2008.
- ↑ For more on the success of smallpox contact tracing, see: McGuire-Wolfe, Christine. Foundations of Infection Control and Prevention. Burlington, MA: Jones & Bartlett Learning, 2018, pg. 11.
- ↑ For more on recent contact tracing technology and application, see: Mittelstadt, Daniel Brent. The Ethics of Biomedical Big Data. New York, NY: Springer Berlin Heidelberg, 2016, pg. 26.